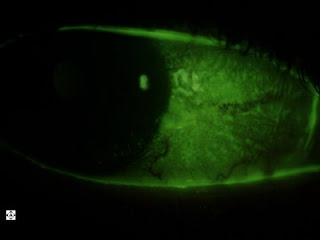
This patient has a "pterygium" on his left eye. This is scar tissue that develops from years of exposure to sunlight, dust and wind. It grows over the cornea with continued exposure and lack of sun protection. This patient's has remained this way for years.

This is the same patient's right lens. A slit of light is shined through the lens, so it's like looking at the lens in cross section, with the left side of it being the front of the lens and the right side being the back of the lens. You can see the layers in it. It's not a cataract unless these layers, usually the center, becomes cloudy. This is pretty normal lookingn.

Below is a photograph of the same patient's right eye with a nevus. The white dots are lipid deposits called "drusen" on the surface of the nevus. A nevus is like a mole in the eye. It just needs to be watched yearly to make sure it doesn't grow.

This is a picture of the same patient's lash ptosis. Most lashes come out or up. His point down. This condition does not bother the patients unless they actually curl into the cornea.