Search Eye Pictures
Tuesday, December 29, 2009
Saturday, December 12, 2009
POST OPERATIVE ABRASION
Very rarely a patient might get a corneal abrasion after cataract surgery. This can come either from a rupture of a bullous keratopathy (which looks like a blister from inflammation that occurs under the outer epithelial layer), or from the eye opening under a pressure patch and being scratched by the patch.

The above photo is the normal left eye with dye in the eye, to stain the tears.
 Here's the abrasion in the right eye the evening of surgery. The patient was in a lot of pain. We put antibiotic ointment in the eye and pressure patched the eye.
Here's the abrasion in the right eye the evening of surgery. The patient was in a lot of pain. We put antibiotic ointment in the eye and pressure patched the eye.
 This is the corneal abrasion the day after surgery. You can see the edges well demarcated. At this point we used a pressure patch, had the patient take antiobiotic drops four times a day, and kept the steroid at a low dose to help with post-op inflammation, without inhibiting wound healing. A delicate balance.
This is the corneal abrasion the day after surgery. You can see the edges well demarcated. At this point we used a pressure patch, had the patient take antiobiotic drops four times a day, and kept the steroid at a low dose to help with post-op inflammation, without inhibiting wound healing. A delicate balance.
The above photo is 4 days after surgery. The epithelium has grown over the abrasion and the edges are now fusing together. The patient will feel a foreign body sensation until this is totally healed. It may take about a week or so until it heals completely, during which time the vision will be blurry. But ultimately this patient will see just as well as if the abrasion never occurred.

The above photo is the normal left eye with dye in the eye, to stain the tears.
 Here's the abrasion in the right eye the evening of surgery. The patient was in a lot of pain. We put antibiotic ointment in the eye and pressure patched the eye.
Here's the abrasion in the right eye the evening of surgery. The patient was in a lot of pain. We put antibiotic ointment in the eye and pressure patched the eye. This is the corneal abrasion the day after surgery. You can see the edges well demarcated. At this point we used a pressure patch, had the patient take antiobiotic drops four times a day, and kept the steroid at a low dose to help with post-op inflammation, without inhibiting wound healing. A delicate balance.
This is the corneal abrasion the day after surgery. You can see the edges well demarcated. At this point we used a pressure patch, had the patient take antiobiotic drops four times a day, and kept the steroid at a low dose to help with post-op inflammation, without inhibiting wound healing. A delicate balance. The above photo is 4 days after surgery. The epithelium has grown over the abrasion and the edges are now fusing together. The patient will feel a foreign body sensation until this is totally healed. It may take about a week or so until it heals completely, during which time the vision will be blurry. But ultimately this patient will see just as well as if the abrasion never occurred.
RESTOR LENS
Wednesday, December 2, 2009
Tuesday, November 24, 2009
Saturday, November 21, 2009
NUCLEAR CATARACT
Thursday, November 5, 2009
Saturday, October 10, 2009
RPE ATROPHY
The subtle yellowish area near the center is an area of RPE atrophy. RPE are the pigment cells under the retinal. This atrophy is in a 56 year old and may be a precursor for macular degeneration. Patient can begin preventive measures against AMD such as diet and exercise changes. Smoking is a big risk factor.


Tuesday, September 29, 2009
Cortical Spoking Cataracts
The top picture is the left eye of a patient and the bottom is the patient's right eye. You can see in the pupil that there is a cortical opacity, greater in the right eye than the left. Interestingly, this patient see's 20/20 in the right eye during the day. But at night the pupils get bigger and the light hits the cataract and causes starbursting of headlights. Very bad in the rain but nice at Christmas time when looking at lights.


Saturday, September 19, 2009
CORTICAL CATARACT
Wednesday, September 16, 2009
INTERESTING BLOOD VESSEL ON IRIS
This is no big deal. It's a blood vessel interwoven into the surface of the iris. It won't cause any problemd for this patient, just an interesting anomoly. The ones that cause concern are new, small blood vessels that can leak in the case of diabetes or other diseases where the eye is not getting enough oxygen.


Monday, September 14, 2009
SNAILTRACK DEGENERATION
The white area is thinning of the peripheral retina called "snailtrack degeneration". There is an increased risk of retinal tears or holes that could then lead to retinal detachment and potential loss of vision. Patient should be seen yearly and watch for floaters, flashes, and shadows in the vision.


Friday, September 11, 2009
TREATED RETINAL TEAR
MACULAR SCAR
The macula is the area of the retina that serves our central vision. This patient has a scar in the center of his left macula (small whitish area in the center of the top picture). The bottom shows his normal right eye macula. Surprisingly, this patient see's 20/20. This kind of scar can come from sun starring when a child. Or there may be other causes. It is unlikely to cause problems in the future for this patient.


Friday, August 28, 2009
Monday, August 17, 2009
RECURRENT CORNEAL EROSION

This patient presented complaining of pain when he woke up one morning. He has also had pain in the eye a couple afternoons. On examination he has this small irregularity just below the pupil on the cornea. This irregularity causes adhesion between the lid and the cornea during sleep and then when waking up the outer protective cells of the cornea come off with the lid, exposing the unprotected layers beneath.
Treatment is usually artificial tears to start with. If that is not enough, then a special ointment at bedtime helps. If that doesn't help, then surgery to flatten the area of the cornea is indicated.
How does the irregularity start to begin with? It can occur from a genetic disorder that causes an irregular corneal surface, or from scarring from a previous injury, or a focal scar from a previous herpes simplex virus infection.
Wednesday, August 12, 2009
Thursday, July 23, 2009
PIGMENTARY DISPERSION

This photo is of what we call "Kruckenburg's Spindle". It's the pigment cells on the back surface of the cornea. It occurs because zonules from the lens of the eye (behind the iris), rub up against the back surface of the iris, and slough off the dark pigment cells, which then float to the front of the eye and attach to the cornea. The cells also go in the "angle" of the eye where fluid drains. If the drain becomes too clogged up, it can cause pressure to rise, increasing the risk for glaucoma (damage to the optic never because of that pressure).
MACULA ON RETINAL DETACHMENT

This is a picture of a retinal detachment. You can see the optic nerve in the center of the photo, but it's hazy for two reasons. First I focused the camera more forward on the detached retina (above), and there's blood in the eye. The detachment is the billowing, whitish membrane you see above. Normally the retina is attached to the back of the eye. There is no vision wherever the retina detaches off the back of the eye. This patient has a "macula-on" detachment which means, if we get this repaired soon enough, he should have most, if not all his central vision restored.
Friday, June 19, 2009
GREAT LASIK FLAP
Friday, June 12, 2009
CHOROIDAL NEVUS AND ANTERIOR CAPSULAR CATARACT
The first picture below is of a choroidal nevus. This is a pigmented area. The white spot on top of it is drusen, which often forms on nevi. This patient will be followed at first on a 6th month basis to make sure it does not progress to melanoma.

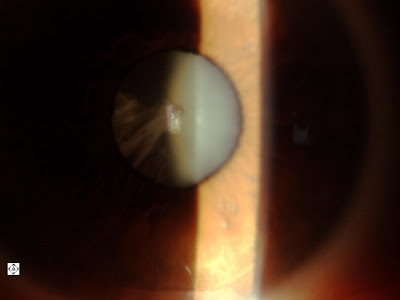
This same patient has an anterior capsular cataract in the right eye. This is a very rare cataract. It does cause some vision decrease, but not enough to justify cataract surgery.

This same patient has an anterior capsular cataract in the right eye. This is a very rare cataract. It does cause some vision decrease, but not enough to justify cataract surgery.
POSTERIOR SUBCAPSULAR CATARACT
Below is the left eye of a patient with a cataract on the back of the lens. The picture on the bottom is of the other eye. This type of cataract can occur spontaneously, or from use of corticosteroids, trauma, or diabetes. It has not yet reached the point where it significantly decreases vision, but this type of cataract has a tendency to grow fairly rapidly and significantly decrease vision at some point.


GLAUCOMA
Below is the right optic nerve in a patient with glaucoma. There is deep cupping when compared with the picture below it of a normal optic nerve. The patient had a visual field test that showed the beginning of vision loss, right eye more so than left. The patient was given drops to lower pressure at least 25% and will return in a few weeks for a follow-up.
Saturday, May 16, 2009
CONTACT LENS OVERWEAR
This patient wears standard disposable contact lenses all day long. You can see from the photos before that there are blood vessels growing into the cornea and inflammation associated with the cornea being starved from oxygen. Solution for this is to get refit in a contact lens that breathes more oxygen and wear glasses more. A little less convenvient but the eyes are worth it! As I've been telling patients lately, we'll go through a lot of cars in our lives but only one set of eyes.


Friday, May 15, 2009
Unusual Cortical Cataract

This is an interesting type of cataract. It is difficult to tell if this is congenital or acquired. Likely it is acquired because you would think and eye doctor would have told the patient about this when he was younger. This cataract does not effect central vision because the central visual axis is still clear. But at night when the pupil dilates, the patient may see haloes and starbursts.
Wednesday, May 13, 2009
CORNEAL ABRASION
Thursday, May 7, 2009
GHOST VESSELS
Friday, May 1, 2009
BLOOD VESSELS GROWING INTO CORNEA FROM EXCESSIVE CONTACT LENS WEAR



The above photos demonstrate blood vessels growing in to the cornea on a patient who wears their contact lenses every waking hour. You can see the redness also around the cornea/conjunctiva margin. These blood vessels grow because of decreased oxygen getting to the cornea. The body tries to compensate by growing blood vessels.
Unfortunately increased blood vessels to the cornea result in increased risk of future immune responses (episodes of redness, pain, inflammation, swelling, light sensitivity, and decreased vision) and also indicate an increased risk for severe corneal infection. These can result in corneal ulcers where the bacteria actually eat away at the cornea. These ulcers are treated aggressively to prevent loss of the eye or loss of vision . They result in permanent scars that, if located centrally, sometimes require a corneal transplant.
I refit this patient in to a lens that breathes about 5 times more oxygen than the standard contact lens. Even so, it is recommended that patients give their eyes a rest from their contact lenses a few hours in the evening and maybe a day or two during the week when possible. LASIK is actually less risky than continuing to wear the same lens the same amount of time.
It is tempting for contact lens patients to overwear their contact lenses either to save money or because of convenience. There are many people who get away with it without insult. However, when serious problems occur, it is almost invariably in those patients who overwear their contact lenses. Either they wear them from the time they get up to the time they go to bed every day, or they sleep in them on a regular basis, or they don't replace them when they're supposed to, or they don't replace their case when they should . Rarely do these individuals have a good pair of glasses that they like.
Wednesday, April 29, 2009
RK and AK scars
Subscribe to:
Posts (Atom)