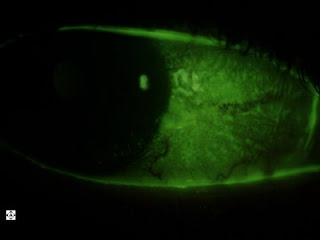
This is an eye with a subconjunctival hemorrahge. A "subconj" hemorrhage is one of the most common eye conditions that brings patients in to the clinic. It appears very scary to the patient when they look in the mirror and see all this blood in the eye.
The reality is that this is one of the least damaging condition for the eye. It does not threaten the eye or the vision and it clears up within a week or so without any treatment. Sometimes there may be some mild discomfort that can be addressed using artificial tears.
So what causes a subconjunctival hemorrhage? Basically it is just a broken blood vessel under the conjunctiva layer of the eye (this is the saran-wrap-like layer over the white part of the eye). These blood vessels are very sensitive and brittle. They can break easily for any reason, or no reason at all. Sometimes lifting something heavy, getting up rapidly, straining, bending over, coughing, sneezing, or low platelet count as may occur on blood thinners can contribute.
If they recur, blood tests can be done to assess the platelet count to make sure the patient is not anemic. That is not necessary on a first time occurence since this is such a common condition that occurs in most people at some point in their lives.